Bimaxillary advancement with complicating factors A case studyPatricia Brinkman-Falter, RDH, MS, COM
Orofacial Myofunctional therapy is an important adjunct to the successful recovery of bimaxillary surgery
Introduction
- Bimaxillary surgery is gaining favor as first treatment for OSA
- Posture is affected because of airway constriction
- No protocol exists for soft tissue recovery
- Often there are craniofacial dystrophies
- TMD can accompany OSA because of parafunctional behaviors
- Diabetes, high blood pressure and rapid breathing are common complicating health factors
Objective
- Identify myofunctional disorders and prepare
musculature and swallow for bimaxillary surgery - Examine post surgical expectations and tools available
to promote overall patient wellness - Identify health conditions that motivate a patient to
pursue bimaxillary surgeryList items go here
History
- Childhood mouth breather, posterior tongue tie, bruxism,
snoring - Orthodontia twice with head gear, four bicuspid
extractions, later ALF and myofunctional therapy - Piper 5 degenerative TMJD, with prior arthrocentesis
- Multiple apneas in REM sleep, fragmented sleep
- Increased heart rate, blood pressure, weight gain,and
retinopathy
Discussions
- Easier aspiration of thin liquids immediately after surgery
- Vocal changes – softer, intonation changed
- Normal swallow was immediately used
- Soft palate was non functional
- Tongue rest posture was much easier
- Increased airway, resulting in better posture, restful sleep
- Less stress on TMJ and surrounding musculature
- Normalized swallow, rest posture and voice quality
- Exercises should be individualized for abilities



Pre Surgery



3 weeks post surgery



3 months post surgery



6 months post surgery



Scientific Poster presented at the 2019 IAOM conference
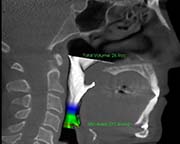
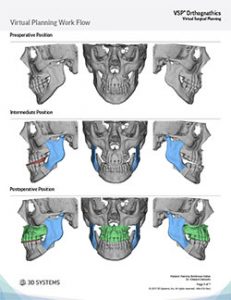
Surgical Plan
Exercises Used
Week 1
Squirt liquids into mouth
Palatal tracing
Hyoid release
Wiggle jaw side to side
Move lips
Trigeminal trace (T-Touch)
Week 2
Add tongue points
Add tongue to spot exercises
Start use of small straws for thin liquids
Week 3
Point and trace combined
Started used of maroon spoon
Tongue on Spot words
Lip smacks
Month 2-3
Start opening jaw with tongue blades
Lymph drainage massage
Coherent breathing
Marshalla’s “Butterfly”
Soft palate/uvula pull
Surprised Turtle
Month 3-6
Soft chew diet
Tongue presses
Singing
Upper cheek toning
Sleep Studies
DESATURATIONS Prior Present
Mean 94 98
Minimum 90 97
Maximum 99 99
PULSE RATE
Mean 77 76
Minimum 56 57
Maximum 113 80
RESPIRATORY INDICES
pRDI 28 0
pAHI 6.3
.25
ODI 3.5 0
